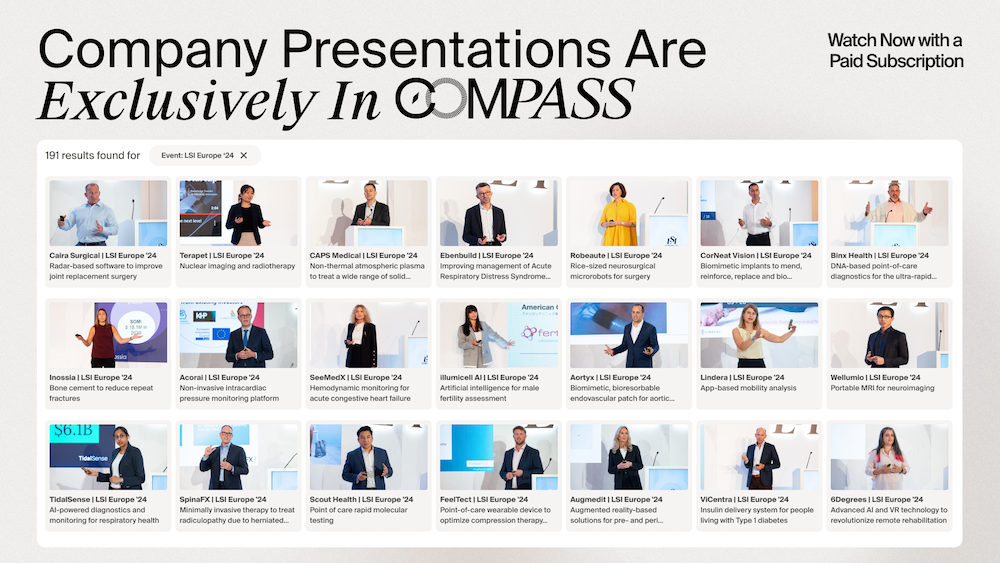
- Video Library
- Steven Mickelsen Presents Field Medical at LSI Europe '23
Steven Mickelsen Presents Field Medical at LSI Europe '23
shaping the future of
Medtech at LSI USA ‘26
Waldorf Astoria, Monarch Beach

Steven Mickelsen
Dedicated to finding new and better treatment options for patients that have challenging cardiovascular problems. My efforts have focused on developing medical devices and technologies that impact treatment of heart rhythm and other important health problems. My inclination is to work on projects where new therapeutic technologies are evolving from the preclinical into the clinical phase while maintaining a presence on the front line of clinical cardiology.
Steven Mickelsen
Dedicated to finding new and better treatment options for patients that have challenging cardiovascular problems. My efforts have focused on developing medical devices and technologies that impact treatment of heart rhythm and other important health problems. My inclination is to work on projects where new therapeutic technologies are evolving from the preclinical into the clinical phase while maintaining a presence on the front line of clinical cardiology.

17011 Beach Blvd, Suite 500 Huntington Beach, CA 92647
714-847-3540© 2026 Life Science Intelligence, Inc., All Rights Reserved. | Privacy Policy