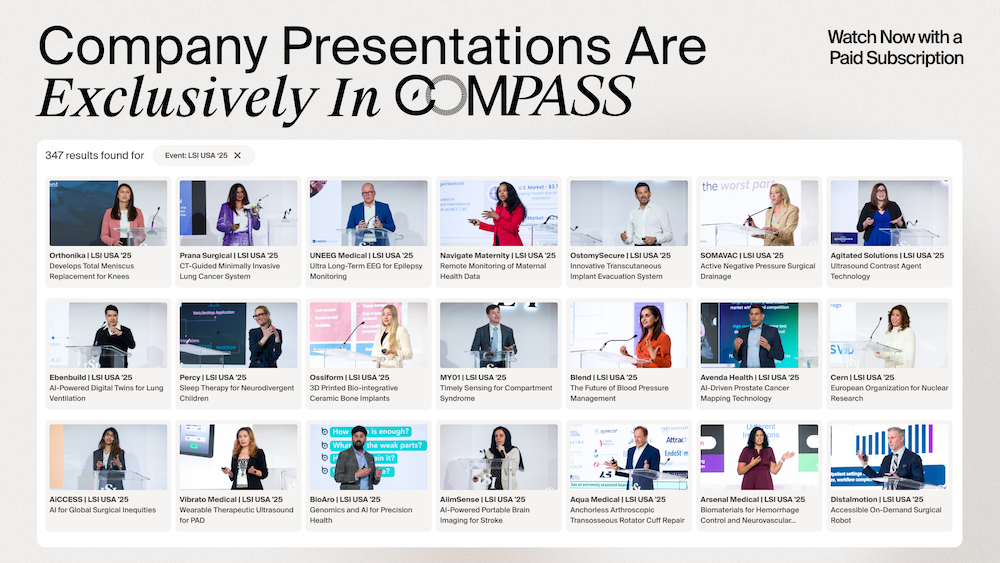
- Video Library
- Paul Molloy, Applaud Medical - Low-Power Ultrasound Lithotripsy System | LSI USA '24
Paul Molloy, Applaud Medical - Low-Power Ultrasound Lithotripsy System | LSI USA '24
shaping the future of
Medtech at LSI USA ‘26
Waldorf Astoria, Monarch Beach
Paul Molloy
Experienced medical device industry CEO and Board Director in public and privately held companies.
Significant global commerce, R&D and operations expertise building teams from ground up to global footprint. Quality and management culture focused. Insightful capital allocation and deployment toolkit for strategic planning and execution. Strong process and project management disciplines towards goal-lines, on time and in budget. Highly credible public market, PE and VC money-raising track record. Close orchestration with investors, banks, funds and analysts to nurture management and investor confidence and alignment. Numerous exits resulting from successful execution of mission. M&A experience including tuck-ins, roll-up, asset sale and purchase and corporate spin-offs and in/out licensing. Several restructuring & turnaround successes. Led one of two IPO's
Paul Molloy
Experienced medical device industry CEO and Board Director in public and privately held companies.
Significant global commerce, R&D and operations expertise building teams from ground up to global footprint. Quality and management culture focused. Insightful capital allocation and deployment toolkit for strategic planning and execution. Strong process and project management disciplines towards goal-lines, on time and in budget. Highly credible public market, PE and VC money-raising track record. Close orchestration with investors, banks, funds and analysts to nurture management and investor confidence and alignment. Numerous exits resulting from successful execution of mission. M&A experience including tuck-ins, roll-up, asset sale and purchase and corporate spin-offs and in/out licensing. Several restructuring & turnaround successes. Led one of two IPO's
17011 Beach Blvd, Suite 500 Huntington Beach, CA 92647
714-847-3540© 2026 Life Science Intelligence, Inc., All Rights Reserved. | Privacy Policy